The Complete Guide to Understanding Back Pain Sciatica
You wake up, your lower back screams in protest, and suddenly, sitting down feels like a marathon.
Welcome to sciatica.
Did you know? The sciatic nerve is the longest in your body, so no wonder it can cause such a fuss.
This article will guide you through what causes that ache, how to spot it, and ways to say goodbye to pain. Ready for relief?
Key Takeaways
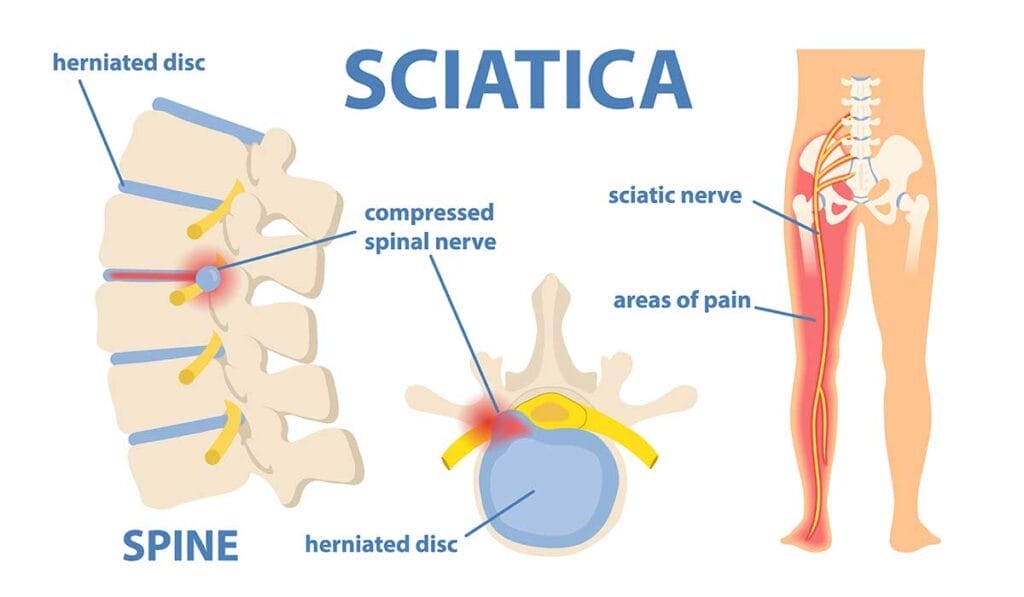
- Sciatica is nerve pain that happens when the sciatic nerve in your lower back gets pinched, often by a herniated disk or bone spur. This causes pain that can travel from your lower back down to your legs.
- Common symptoms include sharp pain, numbness, or tingling in the legs and feet. It can get so bad that sitting or standing feels really uncomfortable.
- You might get sciatica if you lift heavy things the wrong way, sit too much, are overweight, pregnant, or just because of aging and spine problems like spinal stenosis.
- To find out if it’s really sciatica causing trouble, doctors might ask you about your pain and check how you move. They could also use MRI or CT scans to look at your spine more closely.
- Treatments vary but can involve physical therapy exercises to strengthen muscles around the spine and hips, medications to ease inflammation and pain, and surgery for serious cases where other treatments don’t help.
What is Sciatica?

Sciatica is like a bully in back pain, picking on the sciatic nerves that run from your lower spine down each leg. Imagine a garden hose; if you pinch it, water can’t flow smoothly.
Similarly, when these nerves get pinched – often by a herniated disk or bone spurs – they start sending signals of distress.
These are what you feel as sciatica: nerve pain that radiates and can make sitting or standing an adventure in discomfort.
This condition doesn’t discriminate based on age or lifestyle; it can sneak up on anyone who puts too much pressure on their lower back—whether that’s through heavy lifting, prolonged sitting, or just an unlucky twist of fate (like spinal stenosis).
But don’t let sciatica throw you for a loop. With the right approaches—be it physical therapy, medications, or sometimes surgery—you’ve got fighting chances to kick this pain to the curb.
Nerve pain doesn’t have to be the boss of you.
Common Symptoms of Sciatica
Ever felt like your lower back was sending shock waves down to your toes? That might be sciatica talking. This pain doesn’t just stay put in one spot, oh no… it likes to travel from your back all the way through to your legs, making stops at discomfort station and numbness town.
Imagine your leg suddenly deciding to give you a tingle or go numb – not the best feeling when you’re trying to walk, sit, or even just stand there!
Pain that radiates from the lower back to the legs

Feeling a sharp sting zigzagging from your lower back down to your legs? Yep, that’s your sciatic nerve saying hello — and not in a good way.
This kind of pain kicks off in the lower spine area and can shoot right down through your buttocks to the back of one or both legs.
Sciatica is like that uninvited guest at parties who insists on making its presence known, affecting everything from sitting down comfortably to taking a simple stroll around the block.
Now imagine this scenario: You’re bending over to tie your shoe when suddenly — zing! — a bolt of pain travels with lightning speed from your lower spine all the way to your feet.
That’s sciatica showing you it means business. It’s not just about the ache; sometimes you’ll feel pins-and-needles, numbness, or muscle weakness along that path too.
It’s as if someone’s pressing pause on your leg’s normal function, leaving you puzzled and possibly hopping on one foot.
Treating this unwelcome visitor could range from putting ice packs on the affected area to having sessions with a physical therapist or taking medication prescribed by doctors for nerve damage relief.
For some people, treatments might dive into more specialized territory like acupuncture or even surgery when things get serious.
Each step toward managing sciatica—be it changing daily habits or considering spine surgery—is about regaining control over that pesky sciatic nerve without letting it turn into the boss of you and your legs.
Numbness or tingling in the legs or feet

After tackling the discomfort that shoots from your lower spine to your legs, let’s talk about another common buddy of sciatica: that weird numbness or tingle in your legs and feet.
It feels as though they’ve decided to throw a small, uncomfortable party without inviting you.
This sensation isn’t just annoying; it signals nerve irritation or damage somewhere along the line—typically where the sciatic nerve gets pinched.
It’s like stepping on a frozen pond and not feeling the cold through your boots.
Imagine walking around with cotton-stuffed shoes; that’s what people often compare this experience to. Whether it’s pins and needles after sitting too long or a persistent lack of feeling, these are telltale signs not to ignore.
Sometimes, actions as simple as stretching or changing positions don’t shake away that odd sense of wearing invisible socks made of wool woven from discomfort and unease.
Causes and Risk Factors

Did you know some things in your life can make sciatica sneak up on you? Things like lifting heavy stuff the wrong way or not moving around enough can be culprits.
Plus, if carrying a few extra pounds or expecting a baby, those chances might bump up even more.
So, keep an eye out and maybe tweak a few habits—your back will thank you!
Herniated disk
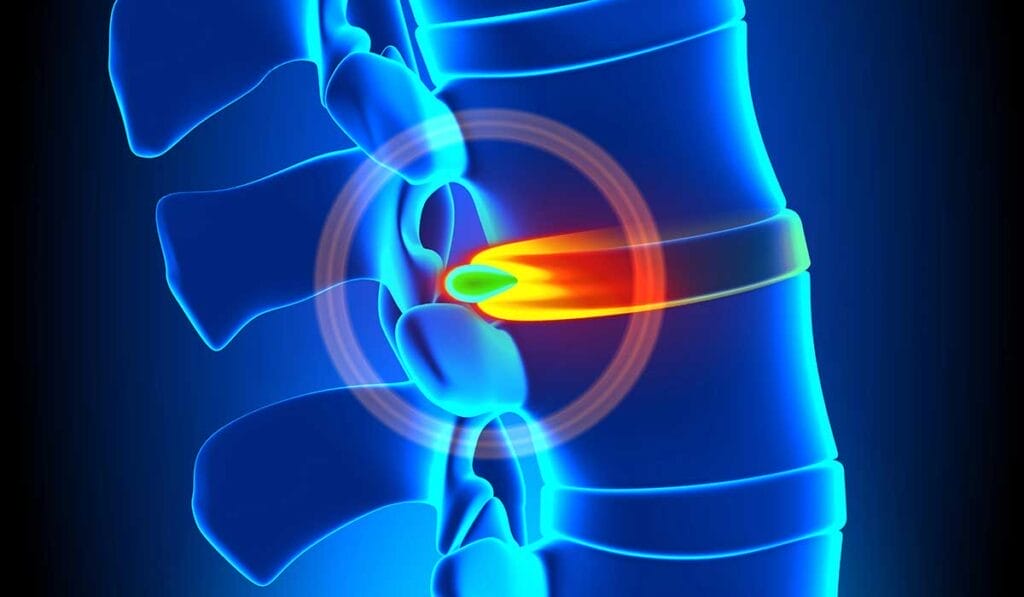
A herniated disk happens when the cushion between your spinal vertebrae pushes out. Think of it like jelly oozing out of a doughnut.
This can tap on nerves, leading to pain that might spread down your lower back into your legs—hello, sciatica! It’s one of those unwelcome guests at the party nobody invited.
Now, imagine lifting something heavy and twisting awkwardly—ouch! That’s often how people end up with a slipped disk. But it’s not just about bad luck; age plays a role too. As you get older, disks dry out and aren’t as flexible.
Add obesity into the mix, and it’s like putting extra pressure on an already squished marshmallow. Not exactly the kind of support you want for your spine.
This brings us to why some folks end up lying flat on their back looking for relief or rushing off to see a specialist hoping for some magic fix. Let’s talk next about another culprit in this saga: spinal stenosis….
Spinal stenosis
Spinal stenosis is like your spine going through a tight squeeze. Imagine the tunnels in your back that nerve roots travel through getting narrower—yep, that’s what happens here.
This narrowing can pinch nerves, leading to pain shooting down your legs or causing clumsiness in foot movements. It’s not a quick hello-and-goodbye kind of pain; it tends to stick around and make itself at home.
This sneaky condition often comes from years of wear and tear on the spine. You could say it’s like an old door hinge getting rusty over time. Things like degenerative disk disease or simply aging can cause these changes…
and let’s not forget about herniated disks adding their two cents into the mix! Even though you might feel more in common with a vintage car than ever before, treatments are available that won’t leave you out for the count.
Facing spinal stenosis? Don’t fret—you’ve got options.
Physical therapy exercises can help strengthen back muscles and take some pressure off those nerves.
For those who need something stronger, medications or even surgery might be on the table to open up space around nerve roots again.
Just because your spine has decided to go ‘narrow-minded’ doesn’t mean you have to put up with discomfort forever.
Pregnancy

Just like spinal stenosis can make you say, “Ouch,” pregnancy might too. Carrying a baby is a beautiful journey, but it’s also one that puts a lot of stress on your lower back. You see, as your belly grows, so does the pressure on your spine and pelvis.
This can pinch nerves in the worst way.
Your body also releases relaxin during pregnancy—a hormone that makes your joints more flexible for childbirth. Sounds helpful, right? Well, sometimes it’s too much of a good thing.
Your pelvis loosens up alright, but this extra flexibility can lead to instability and pain in your lower back and hips. Imagine trying to balance a watermelon while your body insists on playing by different rules every day—that’s pregnancy sciatica for you!
Obesity

Shifting gears from pregnancy, let’s talk about another condition that impacts your spine – being very overweight. Excess pounds put extra pressure on your lower back, leading to sciatic pain.
Think of your spine like a bridge… carrying too much weight can make it harder for the bridge to do its job.
Being overweight often leads to herniated discs and pinched nerves because all that extra weight is just too much for the disks in your spine. It’s like packing too many books into a backpack; eventually, something’s got to give.
And when discs slip or bulge—hello, sciatica! It’s crucial to keep an eye on those scales not just for your waistline but also for your back’s sake.
Diagnostic Approaches

Finding out if it’s sciatica starts with a chat and a check-up. Your doctor will ask about your pain and do some simple tests to see how you move.
They might also take pictures of your back with special cameras, like an MRI or a CT scan, to look closer at what’s going on inside.
This helps them see the big picture and figure out the best way to help you feel better.
Physical examination
Doctors start with a chat about your medical history and then move on to the hands-on stuff during a physical exam. They check how well you can move and pinpoint where it hurts the most.
Think of this as their way of connecting the dots between what you feel and what they see.
Next, they might ask you to walk on your toes or heels. This tests your muscle strength and nerve health from lower back down to your legs, looking for signs of sciatic nerve dysfunction or lumbar radiculopathy—fancy terms for the troublemakers causing that pain in your backside.
It’s like trying to figure out which wire is loose under the hood when your car acts up—you test different parts until you find the problem.
Then comes checking reflexes—those involuntary responses that happen when certain spots are tapped with a small hammer.
Not everyone’s favorite part, but it’s key in finding out if there’s nerve root compression or other issues along your spine.
This step helps doctors decide if further tests like MR neurography or electromyography (EMG) are needed to get a clearer picture of what’s going on inside. So, while it may seem simple, each tap and request to bend or stretch is part of a bigger quest to ease your low back pain and get you moving freely again.
Imaging tests like MRI or CT scans

When investigating delayed lower back pain, getting to the bottom of the issue often means taking a closer look, and that’s where MRI or CT scans are helpful. Think of them as detectives for your spine, searching for clues hidden beneath the surface.
An MRI scan uses powerful magnets and radio waves to create detailed images of your bones and soft tissues. It’s like having X-ray vision that sees through your skin, muscles, and fat right down to the intricate structures of your spine.
This test shines when looking for herniated discs or nerve compression—common villains in the story of sciatica.
On the flip side, a CT scan combines several X-ray images taken from different angles around your body and uses computer processing to create cross-sectional views of your bones and spinal cord.
Picture slicing a loaf of bread; each slice offers a clear view inside without cutting it apart.
While an MRI is top-notch for seeing soft tissues, a CT scan is better at capturing bone details—helpful if there’s suspicion of lumbar spinal stenosis or spondylolisthesis messing with nerve paths.
Armed with this inner snapshot from either an MRI or CT scan, doctors can tailor treatments specifically for you… Now let’s dive into how these insights pave the way for effective treatment strategies.
Treatment Options
If your back’s been bugging you and it feels like the pain is dancing down your leg, help is on the way. From stretching exercises to lying under the knife, there’s a whole menu of options to kick that pain goodbye.
Physical therapy
Physical therapy steps in as a hero for many battling back pain and sciatica. Think of it as your personal coach, guiding you through exercises that strengthen the muscles around your spine and hips.
These aren’t just any workouts – they’re special moves designed to reduce the pressure on your sciatic nerve.
As you embark on this journey, don’t be surprised if cold packs and hot packs become your new best friends. They’re part of the team now, helping soothe those angry nerves. And let’s not forget about massage therapy – it’s like sending love letters to your tight muscles, encouraging them to relax and stop pinching on that poor nerve.
With every stretch and strengthened muscle, you’re one step closer to waving goodbye to that pesky sciatica pain… Now, let’s talk about medications that might help ease the journey even further.
Medications
Dealing with sciatica means sometimes reaching for the medicine cabinet. Over-the-counter pain relievers like ibuprofen and acetaminophen can reduce inflammation and dull the ache.
They’re your go-to buddies when sciatica throws a surprise party in your lower back. But let’s not forget about muscle relaxants. These can help if your back decides to tighten up like someone just told it a really scary story.
For those times when over-the-counter options don’t cut it, doctors might suggest stronger stuff—like steroid injections right into the area that’s singing opera-level high notes of pain.
Imagine telling that pesky inflammation, “You’re not allowed here anymore,” with the authority of a bouncer at an exclusive club.
Next up, let’s bend and stretch our way into physical therapy…
Surgery (in severe cases)

Sometimes, sciatica pain sticks around like an unwanted guest. If physical therapy and medications have waved the white flag, surgery might step in as the hero you didn’t know you needed.
Think of it as a precise operation—not just any kind, but one that targets your lower back pain with superhero precision. The types to talk about are diskectomy or laminectomy, where surgeons play a high-stakes game of remove-the-bad-disc or make-more-room-in-the-spine.
This isn’t a decision made on a whim. Imagine having a chat with your doctor about whether to take this route. They’ll consider how much your back is cramping your style—like if you’re struggling with walking or losing control over bladder functions (yikes!).
Not everyone signs up for this adventure; only severe cases where nerves are waving red flags get backstage passes. And recovery? It’s not overnight magic but think of it as rebooting your system—a process that gradually brings relief from that pesky nerve impingement causing all the trouble down there in leg town.
Additional Comments about Sciatica from Dr. Nguyen
As an aside, through trial and error and evaluating a few hundred sciatica patients in the past few years, I think I have “discovered” the usual cause and, therefore, the solution for sciatica.
Sciatica correlates with buttock muscle weakness since the sciatica nerve originates and travels through the buttock muscle first. 95% of patients with sciatica have a “skinny” or flat butt indicating relative muscle non-development.
In contrast, runners and sprinters, and gym people that focus on leg days have round, firm butts and rarely have back pain or sciatica.
Sciatica can be resolved in most patients within a few weeks. The solution for patients not going to the gym is to perform 100 bodyweight deep squats to strengthen the gluteal muscle.
Gym rats must add weights to the squat, approaching 50% of their body weight, to strengthen their glutes.
The key to the correct form for the squat is to ensure that the buttock starts below the knee to activate the gluteal muscles.
When the squat position begins above the knee, the hamstrings and quads are mostly activated, which won’t help with the sciatica.
Another common reason for sciatica is due to knee pain. 80% of patients with sciatica cannot perform the deep bodyweight squat due to knee pain.
If one cannot squat the buttock below the knee, the buttock muscle never gets used in a daily routine and, therefore, gets weaker with time, leading to sciatica nerve pain.
The solution for the knee pain is simply stretching the knee by maintaining the squat pose just above the knee pain threshold for 30 seconds to 1 minute.
Repeating the deep knee bend stretch several times daily will allow gravity to pull the buttock down and stretch the tight knee ligament.
The knee can be pushed over a week to achieve the goal where the buttock is now below the knee in the deep squat position.
As an interesting historical aside, one theory on the causation and explosion of the incidence of sciatica pain in modern society blames the contemporary toilet.
Undeveloped countries without modern flush toilets use a squat technique for bowel movements and rarely have back pain or sciatica because the gluteal muscle tone is maintained daily with the squat maneuver.
However, with the advent of the modern toilet and chairs, adults rarely have to squat down and, therefore, do not activate the gluteal muscles.
Over time, this leads to gluteal/spinal muscle weakness, which leads to back pain and sciatica pain.
Squats can activate the gluteal muscles once the buttock can be stretched below the knee.
One hundred bodyweight squats where the buttock starts below the knee are performed daily for 2-3 weeks, sufficient for most patients to resolve the sciatica pain.
When the squats cannot fully resolve the sciatica, injecting the 3rd generation PRF with albumin gel has been sufficient to resolve the sciatica pain in the remaining patients who don’t fully respond to exercise.
Sciatica has been resolved in more than 90% of the patients in our clinic.
FAQs
1. What’s the deal with sciatica and back pain?
Sciatica is a rascal, causing lower leg and buttock pain due to issues in your lumbar spine – think of it as a slipped disc or disc herniation in the discs of your spine. It’s like having an electric shock running down your back!
2. Can you spill the beans on what causes sciatica?
Sure thing! Sciatica can be caused by several conditions such as piriformis syndrome, lumbosacral radiculopathy, peripheral neuropathy, cauda equina syndrome or entrapment neuropathy. It’s like these conditions are throwing a wrench into your nerves roots!
3. How do I know if I’ve got this sciatica?
Well, symptoms can vary but common ones include paresthesia (tingling sensation), drop foot (difficulty lifting front part of foot), loss of bladder control and even abdomen discomfort.
4. So how do we kick this sciatic pain to the curb?
Treatment options range from self-care practices to chiropractic care under a skilled chiropractor. For some folks, nonsteroidal anti-inflammatory drugs (NSAIDs) work wonders while others find relief through alternative therapies like biofeedback.
5. Is there anything that can be done for prevention of sciatica?
Absolutely! Regular exercise and proper posture go a long way in keeping our backs healthy – it’s all about treating our spines like royalty!
6. When should I see a doctor for my back pain?
If self-care doesn’t help after two weeks or if you experience severe symptoms such as weakness or loss of movement in legs or bowel/bladder problems – don’t hesitate to call up your doc right away!

